Look at all the options before deciding if self-insurance is right for your organization.
No matter how much analysis they do, or how fit and healthy their workforce appears to be, many senior managers lose sleep over what seems like a risky choice between being self-insured and fully insured.
On the one hand, employers appreciate that self-insurance cuts out premiums, may exempt them from state mandates and requirements, and potentially save them 4 to 6 percent on taxes and assessments. They're also aware that if their health and well-being programs work and the population stays healthy, everyone's budget may benefit.
But on the other hand, they’re concerned by the unpredictability of claims-related costs.
Could level-funding be the answer?
Level-funded self-insurance is a straight-forward, off-the-shelf product that can be a good option for many small and medium-sized companies that want to move to self-insurance. Like a fully-insured plan, it provides cash-flow certainty. But it also includes stop-loss insurance to protect against the impact of big claims.
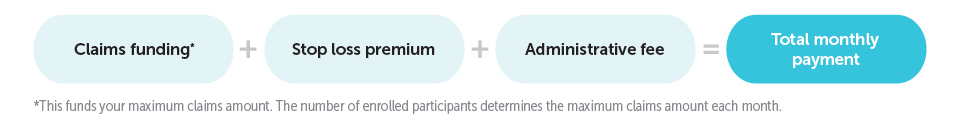
Each month employers pay a “level amount” that includes an administrative fee, stop-loss premium, and an estimated amount for claims, based on a maximum or worst-case scenario. If a company has claims above the estimate, they don’t owe anything additional, and they’re protected by the stop-loss insurance. On the other hand, if the employee population has been healthy and a claims fund surplus exists (and the company has renewed their plan), 50 percent of the surplus is returned to the company during the next year.
What else to consider?
1. Don’t forget the paperwork
Level-funding may sound great, but it’s important to remember that, since it is a form of self-insurance, there are many administrative and compliance implications of switching from a fully-insured arrangement. Many tasks, previously managed by the carrier, now fall to the employer and require a qualified team to work on them. These include:
- Setting privacy boundaries within the company when handling employee health information
- Following specific regulations and having access to legal resources
- Following federal COBRA requirements
- Reporting Minimum Essential Coverage information to the IRS and policyholders
- Deciding how much to charge employees for their coverage
- And, calculating and paying the PCORI (Patient-Centered Outcomes Research Institute) fee.
2. Reduce risk by helping your workforce be healthier
Well-managed health and well-being programs, designed with a specific population’s needs in mind, can measurably improve their health and reduce the risk of claims. Here are some things to think about to have the biggest impact.
- Pinpoint the gaps in your workforce’s health and well-being. Health surveys, assessments and audits will give you a clearer picture of where the biggest health issues lie and which improvements might have the greatest impact. Review health plan utilization trends and audit the work environment. If multiple employees wear eyeglasses, you might offer comprehensive vision benefits. If a high percentage of employees indicate having diabetes, you might offer a diabetes management program and a variety of healthy menu options.
- Take a holistic approach. It’s important to think about behavioral and environmental changes you could drive. If you’re addressing musculoskeletal issues, for example, consider environmental changes like a standing workstation and behavioral changes like a strength training program. If you’re helping expectant mothers, you might offer a maternal health app that helps them stay on track during pregnancy and create a pumping room for moms who plan to pump at work. If you’re addressing mental health, consider adding meditation rooms and starting conversations to stop the stigma around mental health. (Make It OK from HealthPartners is a great resource.)
HealthPartners offers the Balance level-funded product, as well as various health and well-being programs and value-added programs, including: Wellbeats (on-demand fitness), cancer management, healthy pregnancy and virtual coaching.