We're all familiar with headlines about COVID-19 and the flu, but there's a third, lesser-known virus sharing the spotlight, and it's especially tough on young children. RSV, short for respiratory syncytial (sin-SISH-uhl) virus, is an illness that usually causes cold-like symptoms, but can become severe depending on your age and the strength of your immune system.
In a typical year, RSV cases follow the same timeline as the flu – beginning in the fall and hanging around during the colder months when we're often indoors together. In recent years, the virus has made an unusual appearance in the early summer as well, puzzling the medical community. The rise in RSV cases and the proportion of children affected has left many parents with more questions than answers. What is this virus, and is my child at risk?
Below, we provide an overview on RSV — including symptoms, treatment, when to seek medical care, comparisons to other viruses and more.
What is respiratory syncytial virus (RSV)?
RSV is a common virus that affects the lungs and respiratory tract. Most people experience minor, cold-like symptoms and recover on their own with rest and self-care remedies, but it can be more serious for certain groups of people, especially young children and adults over 65.
RSV has been on the rise
RSV usually appears in the fall and winter months, so members of the medical community across the country have been surprised to see a spike in the early summer, too. Experts suspect that relaxed COVID-19 precautions may have led to people having more in-person gatherings and practicing less caution about preventing illness.
RSV is most common among infants and children
RSV commonly affects infants and young children, which is why it's often known as a childhood illness. In fact, nearly every child gets RSV by their second birthday.
However, anyone can contract the virus – so adults should do their best to stay healthy and take precautions to avoid spreading it to others, too.
Those at greatest risk for a severe infection include:
- Babies born prematurely
- Babies under 6 months old
- Young children
- Adults over 65
- People with weakened immune systems
- Those with heart or lung conditions (RSV can also worsen existing heart and lung conditions)
What causes RSV and is it contagious?
RSV is spread through contact with someone who is infected. When the sick person coughs or sneezes, tiny particles of the virus become airborne and can enter your body through your mouth, nose or eyes. It can also live on hard surfaces for hours, so you can get it by touching an object that has virus particles on it.
RSV is very contagious, especially during the week or so that someone is showing symptoms. And it’s possible for some people to remain contagious for up to four weeks.
But if a child or adult has been fever-free for at least 24 hours without the help of fever-reducing medications like ibuprofen and acetaminophen, and if overall symptoms have improved, it’s okay to return to regular activities, including going back to daycare, school or work. Wearing a mask for a few days to a week after returning can help prevent transmitting it to others.
How long does RSV last?
Symptoms of RSV typically last less than a week, and most people are fully recovered within 1-2 weeks. However, those with more serious cases can take longer to recover and may require clinical treatment or hospitalization for trouble breathing or dehydration.
Some schools and childcare centers across the country may ask parents for a doctor’s note or a negative test before their child can go back to school after having RSV, but The American Academy of Pediatrics (AAP) does not advise this. In Minnesota, where we serve many of our patients, the AAP Minnesota chapter explains that RSV tests can remain positive for several weeks after infection, so they shouldn’t be used to test whether someone is cured.
Instead, the AAP recommends following community standard guidelines for returning to school, which we mentioned above. This includes the child being fever-free for at least 24 hours without the help of fever reducers, having no signs of shortness of breath, and general improvement of symptoms. And like other respiratory illnesses, wearing a mask for a while after returning to a group setting can help prevent transmission to others.
RSV symptoms
RSV symptoms can start anywhere from 2-8 days after exposure to a sick person. One way to differentiate it from other cold and flu-like conditions is that RSV symptoms often come in phases, rather than appearing all at once.
Symptoms can include:
- Sore throat
- Cough
- Runny nose
- Headache
- Fever
- Fatigue
- Wheezing
- Sneezing
- Decrease in appetite
Symptoms of severe RSV
Serious cases of RSV can lead to more dangerous conditions, including bronchiolitis (inflammation of the small airways in the lungs) and pneumonia (infection of the lungs). Symptoms of severe RSV include:
- Severe cough
- Difficulty breathing
- Rapid breathing
- Wheezing
- Bluish color to the skin (from lack of oxygen)
Symptoms of RSV in babies
In addition to the symptoms listed above, specific signs of RSV in babies include:
- Increased irritability
- Unusual fatigue
- Poor feeding due to decreased appetite
- Fever
- Pauses in breathing (apnea)
Because babies' immune systems are so new, they haven't developed the strength or immunity to fight off many illnesses. For that reason, infants under 6 months old are at a much higher risk for experiencing a more severe case of RSV.
An added challenge is that babies can't tell us how they're feeling. That's why it's important to watch our littlest ones closely and recognize the signs of illness.
Signs of severe RSV in babies and young children
According to the Centers for Disease Control and Prevention (CDC), RSV is the number one cause of bronchiolitis and pneumonia in children under the age of one in the United States.
Be vigilant in watching for these signs of severe RSV and contact a doctor right away if you notice the following worsening symptoms:
- Difficulty breathing – short, shallow or rapid breaths
- Noticeable pulling in of the chest wall and stomach to breathe (chest retractions)
- Nostrils flaring or head bobbing with each breath
- Short pauses in breathing (apnea)
- Bluish coloring of the skin, lips or fingernails
- Wheezing (a high-pitched sound during inhales can be a sign of bronchiolitis or pneumonia)
- Decreased activity or alertness
- Severe cough
What to do if your child has symptoms of severe RSV
Call your pediatric clinic as soon as possible. Your child's care team can guide you toward the best next steps based on your child's unique symptoms. If you call during business hours, they may advise you to make a same-day appointment or visit your local urgent care. If it's after business hours and your child is having trouble breathing, take them to your chosen emergency room for immediate care.
You can also talk directly with one of our nurses 24/7, 365 days a year, free of charge. They can help you decide if it's time to see a doctor, as well as provide helpful home remedy advice. Call the HealthPartners CareLine℠ at 800-551-0859 or the Park Nicollet Nurse Line at 952-993-4665.
RSV in adults
Older children and adults can also get RSV. Fortunately, their symptoms tend to be milder. Signs of RSV in adults usually include the typical cough, runny nose, sore throat, fatigue and sometimes fever.
Adults over the age of 65 or those with health complications are at higher risk for developing more severe RSV. Serious cases can cause trouble breathing or dehydration and may lead to a hospital stay. RSV usually goes away on its own in a week or two, but if you’re sick longer, or your symptoms are getting worse instead of better, call your primary care doctor right away.
How is RSV different from other viruses?
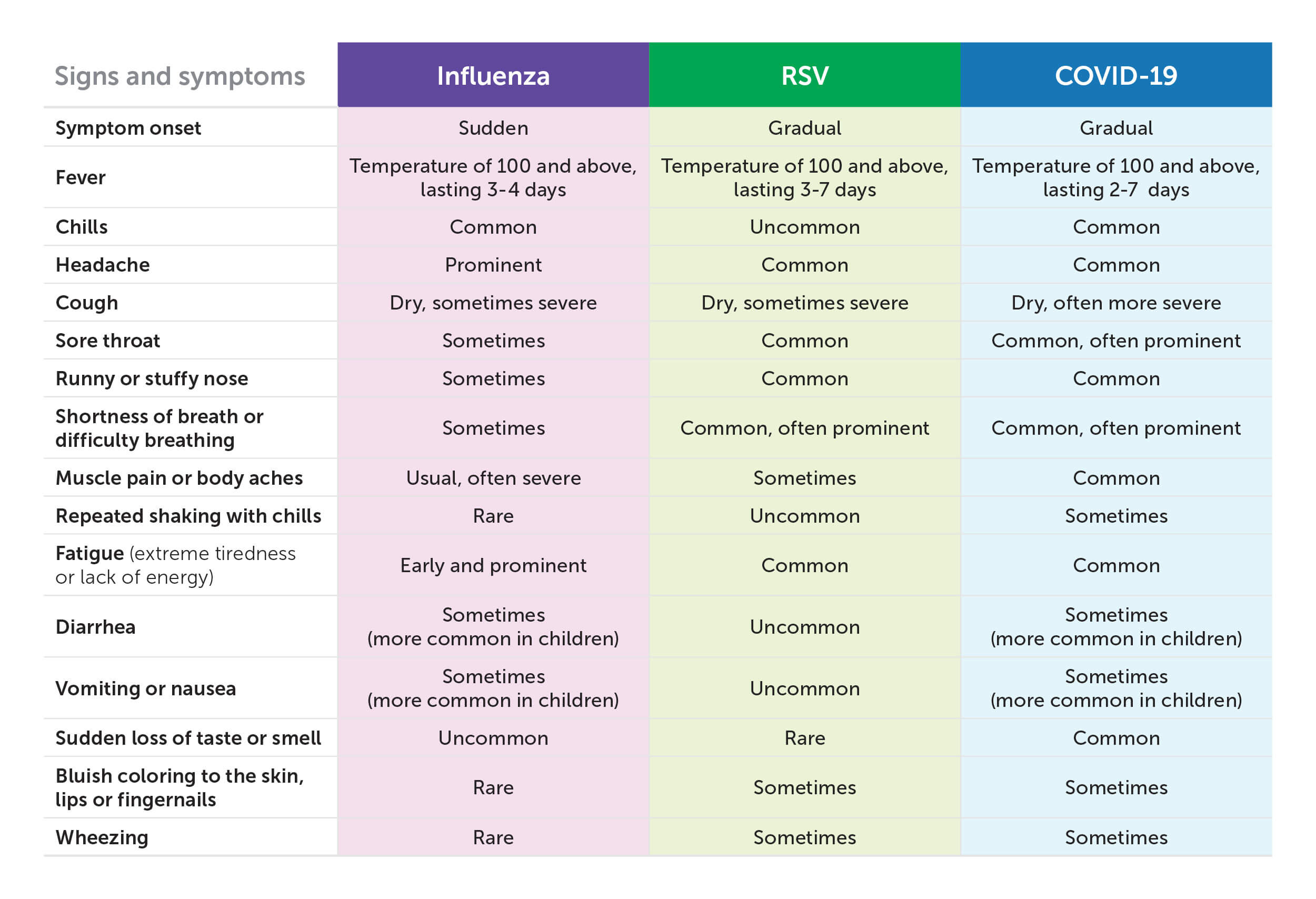
RSV, COVID-19 and influenza (the seasonal flu) are all respiratory viruses with overlapping symptoms. It can be tricky to tell the three apart, so we've created this table to help.
RSV vs. COVID-19
RSV and COVID-19 can be hard to distinguish because they have several respiratory symptoms in common, including cough, shortness of breath, sore throat, fever, headache, fatigue and runny nose.
But people with RSV don't typically experience a sudden loss of taste or smell, or the gastrointestinal symptoms of diarrhea, nausea or vomiting that can occur (especially among children) with COVID-19.
If you or your child are experiencing symptoms of COVID-19 (with or without known exposure), your doctor may recommend getting tested to rule it out.
RSV vs. influenza
RSV and influenza also share overlapping symptoms — including cough, sore throat, fever, headache, fatigue and runny nose — making it hard to know which virus you're dealing with.
One key difference between the two is that symptoms of influenza often appear suddenly, whereas RSV symptoms happen more gradually — and often in phases. Also, like COVID-19, it's common for some people with influenza to have gastrointestinal discomfort, like diarrhea, nausea or vomiting. Those symptoms aren't often seen in children or adults with RSV.
If your symptoms overlap with those of the flu, your doctor may recommend that you or your child get tested for influenza. If you do have the flu, your care team may be able to begin treating you with antiviral medications to help you recover more quickly.
RSV vaccines and other types of RSV protection
The FDA has approved three forms of preventive treatment against severe RSV: a vaccine for older adults, a vaccine for pregnant women and vaccine-like protection for infants and young children under 2. These vaccines can prevent you or your child from severe RSV, but they may not protect against RSV entirely.
RSV vaccine for older adults
The CDC recommends that all adults 60 years of age and older – especially those with chronic health conditions like asthma, COPD or heart disease – get the one-dose RSV vaccine.
If you’re over 60 and interested in learning more about protecting yourself against RSV, it’s easy to get started. You can schedule an in-person or video visit with your primary care doctor to discuss whether the RSV vaccine is right for you and when is the best time to get it.
If you have Medicare Part D coverage, Medicare Part D now fully covers vaccines the CDC recommends for adults, including the RSV vaccine.
The maternal RSV vaccine
The FDA has recently approved a maternal RSV vaccine for pregnant women. This vaccine ensures that babies are protected against RSV the moment they’re born. Your OB-GYN can discuss the vaccine with you at your prenatal visits, and the vaccine itself will be administered between week 32 and week 36 of pregnancy.
If you receive this vaccine at least two weeks prior to birth, your baby will not need the monoclonal antibody treatment we discuss below.
Vaccine-like protection against RSV for infants and young children
Babies can receive a dose of RSV protection in the form of monoclonal antibodies. Where vaccines train the immune system to produce its own defenses against invading viruses, monoclonal antibodies are the defenders, protecting babies’ young immune systems from RSV until they are mature enough to protect themselves.
For the 2023-24 RSV season, we’re offering the antibody treatment – based on availability – only for infants who weigh less than 11 pounds.
Babies born during the typical RSV season (fall to early spring) will usually have their dose at or shortly after birth, and babies born at other times of the year who are about to enter their first RSV season will have theirs in the fall. Children who are at a higher risk of severe RSV can receive an additional dose of monoclonal antibodies before their second RSV season.
Children up to 2 years old with chronic health conditions that put them at a higher risk of severe illness may need monthly doses of a different type of monoclonal antibody throughout the RSV season.
Before the RSV season gets underway in fall and winter, it’s important to receive preventive treatment if you’re eligible. Talk with your doctor to see what is right for you or your child.
Treatment for RSV
While there isn't a treatment for mild to moderate cases of RSV yet, most people recover on their own within a week or two. Here are some home care remedies that can help relieve symptoms and get you on the road to recovery.
- Drink lots of fluids to prevent dehydration.
- Prioritize rest by trying to get extra sleep at night and reducing your daily activities until you're feeling better.
- Take over-the-counter medications for pain relief and to reduce fevers as needed. (Note: Follow your doctor's or your child's pediatrician's guidance on taking over-the-counter medicines. And never give aspirin to children, as it can lead to a disease called Reye's Syndrome.)
- Use saline nasal drops or spray to help loosen a stuffy nose (consult your pediatrician on when this is safe for younger children).
- To help babies breathe easier, use a bulb syringe to remove mucus from their nose.
- Try using steam to improve breathing. To ease dry or stuffy breathing passages, your child's doctor may recommend using a cool mist humidifier in their bedroom at night. If you don't have a humidifier, you can turn on a hot shower with the bathroom door closed to create a steam room effect that can make breathing easier and more comfortable.
For severe cases of RSV that require hospitalization, doctors can provide oxygen and IV fluids, as well as medications or procedures to help open the airways.
How to prevent getting (or spreading) RSV
To help avoid getting or spreading RSV, the CDC and AAP advise practicing the same methods that are recommended to prevent other seasonal illnesses.
- Get vaccinated if you’re eligible – All adults over 60, pregnant women, and children younger than 8 months old can receive preventive treatment from RSV in the form of a vaccination or monoclonal antibodies. Children between 8 months and 2 years old with certain health conditions that put them at higher risk of severe RSV can receive additional monoclonal antibodies.
- Wash your hands frequently – Every time you wash your hands, do so for at least 20 seconds with warm water and soap. If you can't wash your hands, use an alcohol-based hand sanitizer that contains at least 60% alcohol, especially after being in public spaces.
- Avoid touching your eyes, nose and mouth with your hands – Even when you think your hands are fairly clean, try to avoid touching your face, which is a common way for viruses to spread.
- Cover coughs and sneezes – Cough or sneeze into a tissue or the inside of your elbow. (As a fun way to help your child remember to use their elbow, you can encourage them to use their “chicken wing” when coughing or sneezing.)
- Disinfect surfaces – Wipe down commonly used surfaces in your home regularly with a virus-killing disinfectant. It's also a good idea to wipe down cart handles and similar surfaces when you're out shopping.
- Stay home if you're not feeling well (especially if you have a fever) – It's recommended that you or your child stay home if you have a fever, and for at least 24 hours after your fever goes away (without the help of over-the-counter medications). In addition, you or your child’s symptoms should show improvement before returning to school, daycare or other group settings. The AAP advises childcare providers not to require a negative test or a physician’s note for children returning from RSV illness, but to instead follow the community standard illness protocol for kids returning from a respiratory infection.
- Keep a healthy social distance – Stay six feet apart from people in public, or from those you know are sick.
- Avoid touching or kissing babies – It may be tempting to reach out for those tiny fingers, but it's important for babies to stay at a healthy distance from those outside of their immediate family.
Our family medicine and pediatric care experts are experienced in diagnosing and treating RSV, along with many other illnesses.
Do you or your child have RSV-like symptoms? Get the care you need.
Our family medicine and pediatric care experts are experienced in diagnosing and treating RSV, along with many other illnesses.