International development

HealthPartners drives international cooperative health development
HealthPartners was founded as a cooperative in the U.S. in 1957. Since then, we’ve expanded our mission of transforming health care in our own communities to transforming health care internationally. We’ve prioritized making a measurable impact on affordability and accessibility of health care in African countries through the development of cooperative health insurance.
Our innovative approach to cooperative health insurance helps low-income countries increase access to health care while improving the overall quality of care – creating better health for citizens, regardless of their circumstances. HealthPartners International Development carries out the HealthPartners vision of “health as it could be, affordability as it must be, through relationships built on trust” on a global scale via donor funds.
HealthPartners International Development is funded by the Cooperative Development Program (CDP) at the United States Agency for International Development (USAID).
HealthPartners brings cooperative development model to Kenya
The Kenyan government is committed to achieving universal health coverage. The challenge is reaching populations with irregular and unreported income who work outside the formal tax structure.
The Ministry of Health of Kenya requested technical advice from HealthPartners International Development to help them meet the needs of the 73% of their population who have not yet been able to benefit from health insurance.
In October 2023, HealthPartners received a five-year, $8 million grant from the U.S. Agency for International Development (USAID) to assist the government of Kenya health co-op innovations that will meet the health care needs of all Kenyans. Our role in Kenya is to identify solutions and connect partners through sustainable health systems that give members a voice in the cost and quality of their health care.
The HealthPartners approach to international cooperative health care development
Since 1997, we have leveraged our expertise to develop an international health cooperative model in Uganda, as well as further advancement work in Rwanda, Haiti and Madagascar.
The health co-ops we promote are based on existing systems and financed by local stakeholders to help communities in resource-poor areas overcome their health challenges.
In Uganda:
- We trained local stakeholders to identify and meet the health care needs of their communities. Co-op members and health care providers were supported in developing partnerships with measures of accountability.
- We increased health care providers’ capacity to manage health co-op partnerships, which increased access to care and improved health outcomes.
- We educated health care providers and co-op stakeholders in using data to make results-based decisions.
- We focused on access to care for women and vulnerable populations through sustainable health cooperative development strategies.
- We took community-based approaches that led to strong networks between public and private partners, enabling them to meet community needs in ever-changing environments.
- We improved community health outcomes through better access to quality preventive care with more accountability.

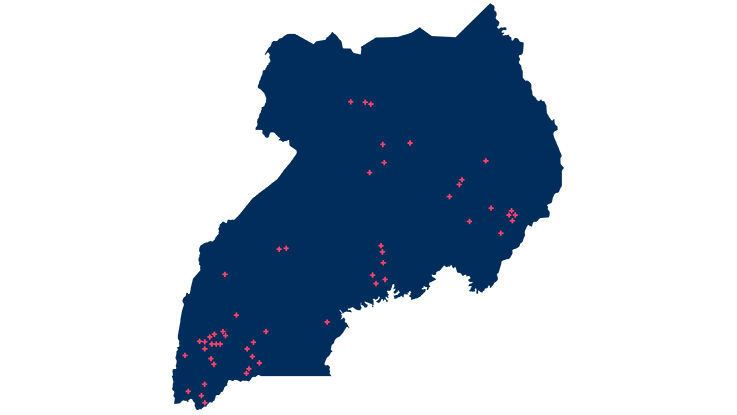
Our cooperative health insurance impact in Uganda
When HealthPartners began work in Uganda in 1997, the health cooperative model did not exist in the nation and no one had heard of health cooperatives – health insurance was only for the rich. Using community-based, cooperative approaches, HealthPartners International Development built strong networks of government ministries, health care stakeholders and communities that made health care accessible and affordable for low-income families.
In Uganda today, there are:
- 29 locally sustainable, member-owned health insurance cooperatives serving 60,000 members
- 70 health care providers offering health insurance using the original HealthPartners cooperative model
Evidence shows that co-op members are in better health and more financially secure than non-members. Health co-op care teams also have better rates of receiving payment for the treatments they provide. HealthPartners helped the Ministry of Trade, Industry and Cooperatives in Uganda draft and adopt seven new policies that guide healthcare cooperative development programs.
After 20 years of network development – from training government regulators to supporting the Ministry of Health and Ministry of Trade, Industry and Cooperatives in adopting policies that regulate and support the development of health cooperatives – HealthPartners is now transitioning our work to the capable hands of our previous staff who have registered their own cooperative development business.
Their nationally registered worker cooperative, Uganda HealthPartners Cooperative (UHPC), is using HealthPartners cooperative development program tools, resources and partnerships to further expand health cooperatives.
What is a health cooperative?
A health cooperative is a health insurance option that is owned and democratically controlled by its members – doctors and patients in cooperation. Health cooperatives make shared risk possible by spreading the cost of care across all members. Due to the power of numbers, the cooperative can negotiate with care providers for high-quality, affordable and low-cost care, as well as benefit packages that meet their needs.
Members of the co-op pay membership fees and quarterly premiums, and a co-pay is due when they receive care. Co-op care teams use the premiums to keep a good supply of medicine and to pay the staff on time. Both measures help improve the quality of care that patients receive.
