Health care cost management
Health care cost management that doesn’t slow your business down
When health care costs go up and start to strain your bottom line, it can be hard to see where you can find value. That’s why our health insurance plans focus on smarter investment in health, not just more.
We do this through fully integrated health, dental and pharmacy plan designs that emphasize total cost of care (TCOC). That means focusing on cost savings by looking at the bigger picture of health and connecting dots across the individual parts of a member’s health journey. In other words, we prioritize targeting and encouraging the right care at the right moment, personalizing solutions to your business’s and your employees’ evolving needs, and driving member engagement with their plan that outpaces the industry standard.
The result? A more health-conscious, motivated and productive workforce. Because we know that when employees are healthier, they’re not the only ones who win – your company does too.
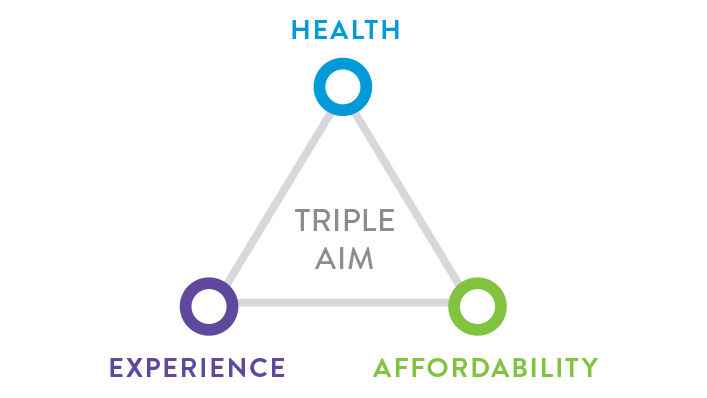
Bringing the “Triple Aim” together: Health, Affordability and Experience
We’re a nonprofit health organization with mission-driven insurance plans that combine our expertise in award-winning care, personalized plans and innovative research. It’s how we collaborate and connect to improve quality and lower costs without compromising care.

A TCOC approach that controls health care costs differently
Managing total cost of care isn’t new, but our approach to TCOC is different. We look beyond what health care claims cost and how to make them less expensive. Instead, we also look at the resources being used to see if they can be used more wisely.
What we’ve learned from our TCOC approach is simple but important: It’s easier (and more cost effective) to prevent medical issues before they need more serious attention. We’re resetting the conversation about costs by aiming to:
- Reduce the volume of care needed – We identify and redirect higher-risk health populations through a combination of our proprietary tools and engaging outreach. We aim to help prevent medical issues from becoming more serious, which in turn helps keep members healthy, productive and happy (and helps keep employer budgets on track).
- Reduce intensity of care – Another part of our population management strategy is to steward employees’ health so they’re less likely to need more expensive care. But when that kind of care is needed (like at the hospital), we also make sure employees have the support they need through personalized disease and case management so they can get healthier sooner. It’s an approach that focuses on the patient while also endeavoring to reduce costs across the board.
How do we accomplish this? Through proactive health monitoring, outreach and engagement with both our providers and members. We don’t just focus on negotiating the cheapest reimbursement rates; instead, we focus on the whole person to create real value, for everyone, at every point.

Learn more about our independently proven cost management model
Our goal is to make health care more affordable for everyone without sacrificing quality or experience. Our full-population, person-centered TCOC model accounts for:
- Member liability and plan payments
- 100% of care provided to a member
- All care, service sites, treatment costs and provider types
- All illness burden-adjusted costs, including primary care, specialty care, pharmacy medication, hospital care and more
- A provider’s price, resource use and efficiency
When all this comes together, we can focus on the overall cost of care by identifying and comparing price, resource use and utilization drivers based on population, provider, condition, patient and procedure levels. We can also build provider contracts based on value, shared savings and risk models, where care systems that deliver exceptional cost and quality are rewarded. That’s why we use TCOC measurements for:
- Patient-centered innovations
- Data analysis to support improvements
- Reporting transparency
- Network configuration
- Integrated health management using a well-being approach
- Clinical support by medical directors
- Provider consultation, contracting and collaboration
- And more
In fact, our measures of TCOC and resource use are one of only two measures of their kind to be endorsed by the National Quality Forum (NQF), and the TCOC metrics we’ve developed are used by over 300 licensees in over 40 states. Why? Because they work.
Learn more about health care cost management
How to proactively manage employee population health and well-being What's total cost of care and how could it help your business? Three tips for employers on how to reduce health care costs without sacrificing quality of care How much group health insurance costs: What every employer should know Read more about total cost of care (TCOC)
